Yesterday I posted about some parenting stuff in the age of Corona Virus. Today we had our first Sunday service after the World Health Organisation declared a pandemic and the Australian Government brought in social distancing measures to limit large gatherings.
We aren’t a large gathering, but our congregation meets in a facility we share with multiple congregations, including one made up of a substantial number of people in high risk categories. It’s a building we don’t operate, so our ability to conduct appropriate cleaning measures between uses is limited.
I’m convinced churches need to participate in flattening the curve, even if our gatherings aren’t large, I think we have a responsibility to love our neighbours, especially the vulnerable. I’m struck by how wrong this can go — Patient 31 in South Korea was an individual responsible for a drastic uptick in Corona Virus infections because of her participation in church events.
I’m convinced that we should act ahead of government advice. The call from Jesus to “love our neighbours” comes with the caveat “as we love ourselves” — it’s important that we be healthy so that we can be in a position to provide good care to others. We want to make it as easy as possible for people to opt out of our service, to non-anxiously (or anxiously) self isolate, without judgment, from this point on. Even if the government doesn’t step in to limit interactions for weeks or months (probably until winter).
I found Andy Crouch’s piece on love in the time of Corona Virus profoundly helpful (I also linked to it yesterday). I’m convinced that we need to find ways not just to virtually connect as church, but to keep meeting together. But this requires careful management of physical spaces and personal hygiene, and our circumstances with our building and the other congregations that meet there mean we’ll probably be encouraging small groups to meet together during our church broadcasts, and to find ways to care for and support one another.
I’m convinced that we need to be prepared, and careful, so that we can love our neighbours well in this time of crisis as a faithful presence in the world — a people committed to taking up our cross and following Jesus. I’m struck by what’s happening in Italy, where hospitals are confronted with making treatment decisions that will determine who lives and who dies. Here’s a quote from a journal article I filed away once for a time such as this.
“Medicine involves faithful presence to those in pain, even—perhaps especially—when hopes for “cure” prove illusory and the provision of care throughout a longer or a shorter span of life becomes the sum of what medicine can offer. This is no easy task. Our helplessness to effect a hoped-for cure can too easily turn to hatred: hatred of sufferers for failing to get well and of ourselves for failing to make them better. In the face of this temptation to impotent rage and to the punitive abandonment of the sick and suffering, medicine needs the church, whose experience of the faithful presence of God in the midst of suffering undergirds its own willingness faithfully to be present to the sick. Only so can the hospital—and the practice of medicine more generally—be, in Hauerwas’ words, “a house of hospitality along the way of our journey with finitude . . . a sign that we will not abandon those who have become ill simply because they are currently suffering the sign of that finitude” (Hauerwas, 1986, 81–2). If anything, Hauerwas may have understated the dependence of the practice of medicine, thus defined, upon the moral community that is the church. In a recent monograph, historian Andrew Crislip (2005) links the emergence of the hospital in the late antique period to the health care system of Christian monasticism. According to Crislip, monastic health care stood in stark contrast to pagan health care in its commitment to care for the crippled, the infirm elderly, and the chronically and terminally ill (Crislip, 2005, 9). “It was standard among ancient physicians at all times to reject chronic or hopeless cases. To treat a patient he could not cure would only diminish the doctor’s reputation, even if it might enrich him somewhat” (Crislip, 2005, 114). Thus, where pagan medicine emphasized prognosis, which allowed the physician to identify hopeless cases and refuse to take them, monastic medicine emphasized diagnosis, which allowed for appropriate healing and caring measures to be taken on behalf of any sufferer (Crislip, 2005, 18–9). There is, in other words, no abstract discipline called “medicine” that offers nonstigmatizing, compassionate care throughout the life cycle. In the West, at least, such medicine originated in specifically Christian communities and was undergirded by specifically Christian moral commitments
M.K Peterson, ‘Salvation and Health: Why the Church Needs Psychotherapy,’ Christian Bioethics, 17.3, (2011), 277-298
Get that — before universal health care in western countries; in the Roman world; doctors would treat people based on who they’d boost their stats from, and who would make them the most money. Christianity turned that on its head because Christians kept caring for vulnerable people, and thus, the modern hospital was born. In the third century AD, a Roman emperor who hated the spread of Christianity, Julian, wrote a letter where he gave an account for the popularity of the religion of the ‘impious Galileans’ amongst the people of Rome. He gave instructions for the creation of something like the modern hospital.
“Erect many hostels, one in each city, in order that strangers may enjoy my kindness, not only those of our own faith but also of others whosoever is in want of money. I have just been devising a plan by which you will be able to get supplies. For I have ordered that every year throughout all Galatia 30,000 modii of grain and 60,000 pints of wine shall be provided. The fifth part of these I order to be expended on the poor who serve the priests, and the rest must be distributed from me to strangers and beggars. For it is disgraceful when no Jew is a beggar and the impious Galileans support our poor in addition to their own; everyone is able to see that our coreligionists are in want of aid from us.”
Here are some steps we’re taking and the way we’re approaching decisions around Corona Virus. I’d love to hear what you’re doing.
- I’ve put together something of a crisis team, this team includes a few well positioned medical professionals, including one doctor in our congregation who is a medical advisor for a senator, and two GPs, but also our small group leaders, kids church coordinator, committee of management and elders. We’re discussing steps to take, and this group will allow us to make decisions quickly as information comes to hand. It’s really important that Christians, who are people of truth, build our decisions and our attempts to be wise, and to love our neighbours, from the truth. So good data and information is really key — both receiving it, making decisions from it, and sharing it — but doing so non-anxiously (again, see Crouch’s article). I’m also an asthmatic, which is a personal risk for me, but one our church leadership team needs to manage too. It’s probably a good thing for pastors of churches coordinating crisis management to make sure their own risk factors are known and that work arounds are possible.
- We’re communicating regularly to our congregation via our Facebook group, and looking at how to communicate to those not on Facebook.
- We’ve asked those who are sick or symptomatic, or potentially exposed, to self isolate, and to let us know so that we can care for them.
- We recognise that meeting together is vital for the Christian life, and loneliness is deadly, and social isolation has the potential to undermine our spiritual and emotional well being, so are working at solutions (in line with the Crouch article, and this useful document he linked). Our small groups, meeting in homes where some of the tips in that document will be easier to manage, will be part of continuity of community and care during this time. Even those groups can embrace technology — various members of our Growth Group have face timed in for weeks where they couldn’t make it already this year.
- We’ve been preaching through Luke’s Gospel, and today were reminded, as Peter denied Jesus, of Jesus’ call for his disciples to take up their cross and follow him. We broke up into small groups to talk about what this might look like during the pandemic. It’s interesting that the quote from the journal article above uses the phrase ‘faithful presence’ — this is common language for us as a church, the idea that this is our calling, along with the idea of a faithful presence being a non-anxious presence because our hope is secure.
- Meals together have been a feature of our gatherings since the beginning. We’re not catering for post-service community lunches during the pandemic, but are instead encouraging people to eat at nearby restaurants (or go home) to avoid handling food/cross contamination.
- We are providing soap and sanitiser on site for people to wash their hands as they arrive. Ideally, we’d be wiping down surfaces and equipment before and after use (we are doing that for our bits and pieces, but there’s uncertainty about which groups that use our facilities use what).
- We’re encouraging parents to make decisions about how to approach church with kids; whether they sit in family groups practicing some reasonable social distancing in our facility, or sending them to kids church and managing hand washing. Again, we want to make it as easy as possible for people to opt out to flatten the curve, while still belonging to and participating in our community.
- Today we ran our first ‘online’ service using Zoom. We’ve got access to a paid account, but like Zoom because should we move to totally online services we want multiple people to be able to contribute to the service. I sticky taped my phone to a mic stand. It worked.

- Presbyterians aren’t typically ‘every week’ communion/Lord’s Supper types here in Australia, but we’re changing our practices to minimise handling of the bread by those preparing it, and we don’t share a common cup (we have little cups of grape juice).
- On the home front, we’ve been doing some careful preparations, putting together a dry food supply that will last us through a period of isolation, but that will also allow us to meet the needs of others. We’ve started freezing meals in containers labelled with their ingredients (to manage intolerances) so that we can share these with those in need.
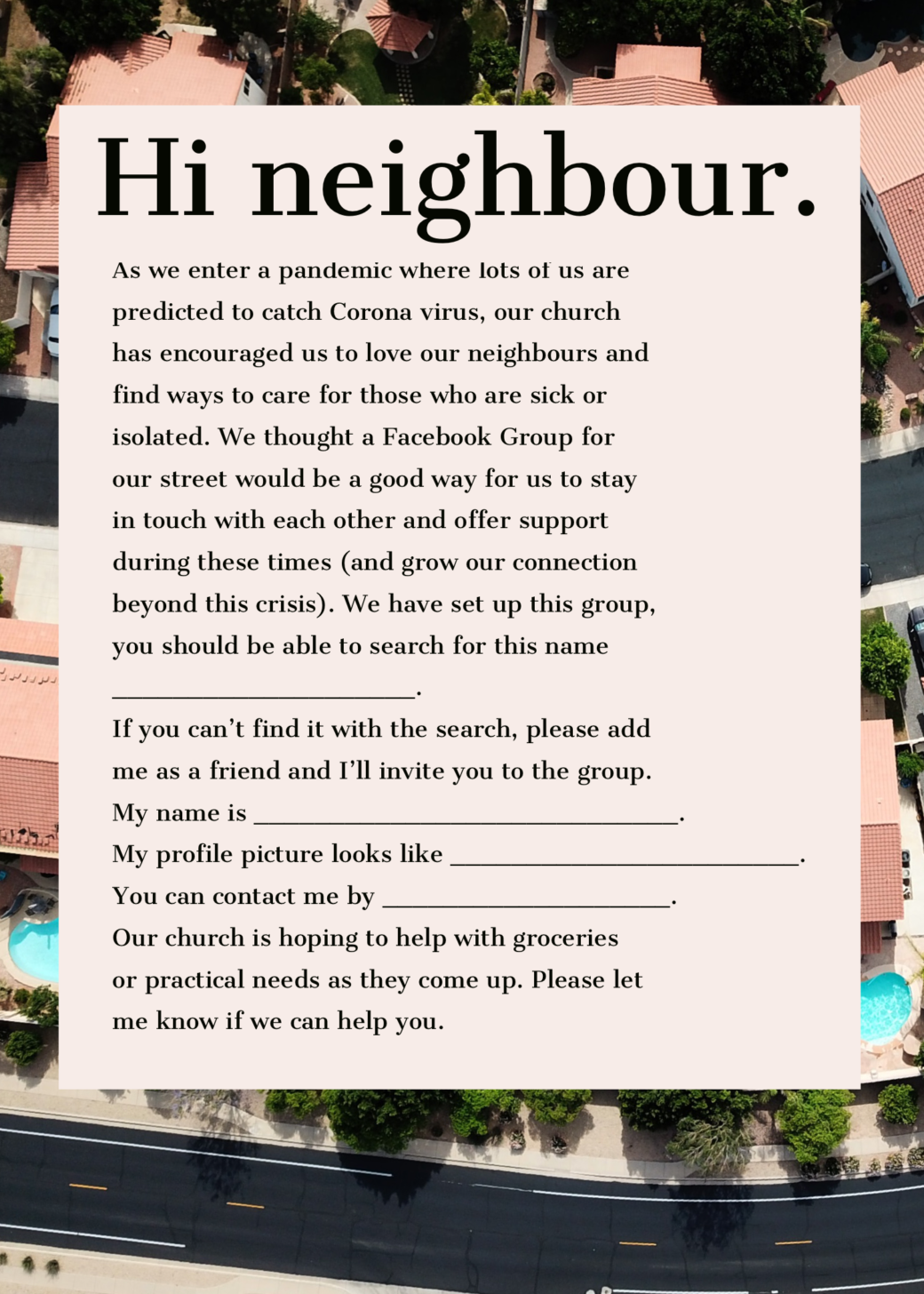
- Our street already has a thriving Facebook group, but people in our church liked the idea so I’ve knocked up this postcard template (pictured below) they can print off using a photo printing service (or their printer) to drop in to neighbour’s letterboxes. Feel free to shameless steal it. The text is (for those who might want to easily adapt/print using word:
Hi neighbour,
As we enter a pandemic where lots of us are predicted to catch Corona Virus, our church has encouraged us to love our neighbours and to find ways to care for those who are sick or isolated.
We thought a Facebook Group for our street would be a good way for us to stay in touch with each other and offer support during these times (and grow our connection beyond this crisis). We have set up this group, you should be able to search for this name ______________.
If you can’t find it with the search, please add me as a friend and I’ll invite you to the group. My name is _________. My profile picture looks like _____________. You can contact me by ______________. Our church is hoping to help with groceries or practical needs as they come up. Please let me know if we can help you. - There’ll be an economic impact of Corona Virus as well as a health one; people in church congregations will be facing uncertain employment situations or losing their jobs, in a bad economic climate. We need to risk manage that as churches with our own budgets, but also want to be in a position to be caring for those affected. This is tricky, but it’s something I’ve flagged with our management team and the crisis management group to be part of our conversation. Another church I follow online mentioned maintaining giving during lockdowns as a good way to care for church staff, and to sustain the church’s ability to serve the community. I thought they did this well.
Over to you — hit us up in the comments on this post, or discussion on Facebook, to let us know what your church is doing, or things we’ve missed.